HMSA pre-authorization policy delaying critical tests, some doctors say
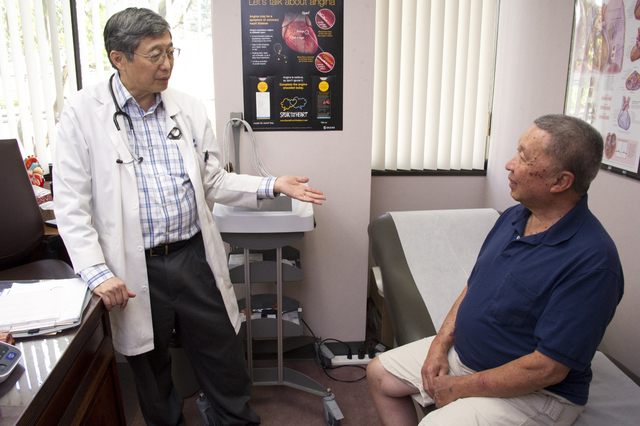
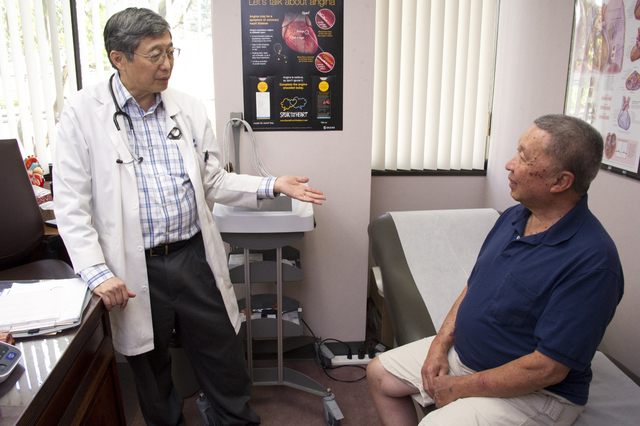
CRAIG T. KOJIMA / CKOJIMA@STARADVERTISER.COM
Dr. Calvin Wong consulted Tuesday with patient Franklin Young at the Queen’s Medical Center.
CRAIG T. KOJIMA / CKOJIMA@STARADVERTISER.COM
Dr. Calvin Wong at Queen’s Hospital.
Jerome Fukuhara knew something was wrong with his heart when it got harder and harder to breathe while walking around the block.
In February the 52-year-old Salt Lake resident went to his doctor, who wanted him to get a heart scan to check for blockages in his arteries. The doctor’s request for a test was denied by the Hawaii Medical Service Association, the state’s largest health insurer, which began requiring pre-authorization on imaging tests in December.
Then in March, Fukuhara had a follow-up with the doctor, who told him to go to the emergency room to get the exam done immediately. HMSA does not require pre-authorization for emergency room or hospital patients. Fukuhara’s test revealed one of his arteries was nearly 100 percent blocked, two others were 90 percent obstructed and a fourth was 80 percent closed. Four days after the test, he was undergoing quadruple bypass heart surgery.
“If I had waited for approval, he’d be dead,” said Fukuhara’s doctor, Dr. Calvin Wong, chief of cardiology at the Queen’s Medical Center.
HMSA said its new pre-authorization policy did not cause a delay in Fukuhara getting the care he needed. The insurer contends that Wong did not submit the medical records required to get the heart scan approved, did not tell HMSA the test was urgent and did not take advantage of an appeal process in a timely manner.
Doctors cite delays
Don't miss out on what's happening!
Stay in touch with breaking news, as it happens, conveniently in your email inbox. It's FREE!
However, the new pre-authorization policy has stirred opposition from many Hawaii doctors who say it is delaying critical imaging tests, resulting in harmful consequences for patients.
HMSA on Dec. 1 began requiring the roughly 3,000 physicians in its network to go through National Imaging Associates Inc., a subsidiary of Scottsdale, Ariz.-based Magellan Health Inc., to approve diagnostic exams — including MRIs, computerized tomography (CT) scans and other cardiac-related procedures — for its 720,000 members.
Previously, HMSA gave most Hawaii doctors a waiver, known as a gold card, that allowed them to skip the pre-authorization process. Physicians with gold cards could order an exam for a patient and get it done within a few days. Now doctors say many of their requests are initially denied and that “standard” appeals can take up to 30 days. HMSA said the average time for pre-approvals is 24 hours once all the necessary information is submitted by the doctor.
To help speed pre-authorization in urgent cases, HMSA revised its December policy, notifying physicians via email Feb. 22 that it would issue “immediate approval” for tests if doctors attest that the case is clinically urgent.
‘The hassle factor’
The fact remains that pre-authorization does delay outpatient testing.
“It’s the process that’s the killer,” Wong said. “They (HMSA) overwhelmed us with the process. I get 10 to 25 pre-authorizations a week. In cardiology everything is urgent. Everybody is a time bomb, and I don’t know when the time bomb is going to explode.”
Wong did eventually appeal Fukuhara’s case, sending HMSA 24 pages of clinical records. Upon receiving the documents, Fukuhara’s test was approved, but by then he had already checked in at the emergency room.
The Hawaii Medical Association, a trade group representing 1,900 physicians, is calling for the immediate suspension of the pre-authorization program. State lawmakers have also taken up the issue. House Bill 2740 would make HMSA legally responsible for deaths or other harm as a result of undue delays in testing. The bill is scheduled to be debated in conference committee today.
Dr. Christopher Marsh, a Honolulu internist, said doctors should have the authority to order tests immediately. “We have technology that’s so good, it’s crazy not to apply it. … We’re in the trenches. We’re on the line, but we have to get approval and run things by a panel of people we don’t even know who haven’t seen a sick person for a while. These guys don’t know what the hell they’re doing. It’s the hassle factor.”
Marsh said his Honolulu practice employs 10 staff to do the administrative work for two doctors.
“They are on the phone or the fax all day long trying to get our patients approved medications, imaging tests, referrals, etc.,” he said. “My beef is that this micromanaging of my day-to-day patient care is trashing my ability to take care of my sick patients.”
Dr. Jon Graham, a neurosurgeon at Queen’s, added, “They’re practicing medicine without a license by having guys on the mainland telling us how we should treat our patients, and yet if we get bad results, we’re liable. These people are telling us how to treat patients without even examining them. If I got a patient with a brain tumor and want to get a follow-up scan to see how much of the tumor is left, I have to get approval. It delays care and it delays treatment. It’s ridiculous.”
National Imaging Associates, the company that reviews pre-approval cases for HMSA, said on its website that it employs board-certified physicians and decides 450,000 requests a month from doctors around the country. NIA’s website said the company offers its clients “industry-leading clinical, operational, and financial resources that allow us to achieve bottom-line results and guarantee multi-year cost savings.” NIA didn’t respond when asked to comment for this story.
‘Put the brakes on’
Not all physicians think pre-authorization is unwarranted.
Dr. John Cogan, a cardiologist and clinical professor of medicine at the University of Hawaii’s John A. Burns School of Medicine, said prior authorization is necessary to safeguard patients and “because physicians do not police themselves.”
“There are physicians in every specialty that order tests inappropriately and do procedures inappropriately,” Cogan said. “Unfortunately, there are physicians that do not practice evidence-based medicine, who look for ways to increase income from doing tests that are moderately appropriate. They get the money from the tests (done in their offices). Since doctors don’t put the brakes on what they’re doing themselves, that is exactly why insurance companies feel they must do it. The insurance companies by default are practicing medicine.”
Cogan said the pre-approval process is tedious and costs him roughly $50 a patient, but he’s never had a legitimate test turned down once the correct information was submitted to the insurer.
HMSA said in an email, “Protecting the health and safety of our members is HMSA’s top priority. Our advanced imaging preauthorization program follows national guidelines developed by top physicians across the country.” When the policy was introduced, the insurer said pre-approvals would reduce unnecessary procedures, avoid patients being exposed to excessive radiation and reduce costs.
HMSA did not respond to the Star-Advertiser when asked:
>> How many pre-authorization requests has HMSA denied?
>> How much money has the policy saved HMSA?
>> Is HMSA tracking what happens to patients who are denied tests?
“Any decision that a doctor or patient does not agree with can be reconsidered,” HMSA said in its email. “This has happened with about 6 percent of these cases. … Just over half of these were overturned and were always the result of receiving the needed clinical information from the physician. We continually evaluate this program based on the feedback from physicians and patients.”
The company said the feedback has already led to several improvements including dedicated phone lines for doctor-to-doctor conversations, expanded hours to accommodate Hawaii physicians and the creation of a local physician advisory panel.
‘It’s overwhelming’
In Fukuhara’s case, Wong requested a “non-urgent” pre-authorization Feb. 12, according to HMSA’s records. National Imaging Associates tried unsuccessfully to let Wong know he needed to submit medical records with the pre-authorization, the insurer said. Wong said his office sent the documents by fax Feb. 15. NIA says it only received the fax cover and denied approval because it still hadn’t received the clinical information.
Wong said he did not contact HMSA or NIA again until after Fukuhara returned to his office for a follow-up visit March 2 and his symptoms had worsened. The next day, Wong appealed the denial of the heart scan. The delay in appealing the original HMSA denial was due to the added work his office has taken on due to the pre-authorization policy, he said.
“It’s overwhelming,” Wong said. “There are so many hoops you’ve got to jump through. We just don’t have the time. It’s a tremendous hassle factor. Everybody I talk to has the same problem.”
Fukuhara checked into the emergency room March 3, and the next day was given the nuclear heart scan, 22 days after his doctor determined he needed one. On March 5, Fukuhara had a cardiac catheterization, a procedure used to diagnose heart conditions, and on March 7 he had quadruple bypass surgery.
When Fukuhara returned home from the hospital March 12, he found letters from both HMSA and National Imaging Associates, dated March 4 and March 3 respectively, notifying him that an appeal had been approved.
“It was too late. I already had the bypass surgery,” Fukuhara said. “I couldn’t understand why HMSA (initially) denied the test. If they looked at what they’ve been paying for in the past 11 years for me medically, they would’ve seen that I’m a high-risk patient. If the cardiologist who I’ve been seeing for 11 years on a regular basis orders a test, there’s a reason. I don’t understand how they expect to save money doing this.”
Physician warned
When the Star-Advertiser asked HMSA about the Fukuhara case and another involving pre-authorization, the insurer’s attorney, Paul Alston, sent a letter to Wong stating that his requests were initially denied because they lacked clinical information, and once that information was sent, the denials were reversed. In Fukuhara’s case, “once that information was submitted — this time as an expedited request — approval was given in 27 minutes,” Alston wrote.
Alston then warned Wong about the steps HMSA could take if the doctor continued to insist that the delay of test approvals was harming patients.
“HMSA has asked that we tell you that — to a certainty — any implication that those patients were harmed by HMSA’s preauthorization requirements is false and defamatory,” Alston wrote. “If you do not immediately notify the media that these allegations are false, you (and anyone else involved in disseminating these false claims) will cause serious reputational harm to HMSA. Please be aware that HMSA is prepared to pursue its legal remedies to address the harm caused by publication of these claims.”
Hawaii doctors aren’t the only physicians unhappy about pre-approval policies.
The American Medical Association, the nation’s largest organization of physicians, conducted a survey in 2010 that showed 78 percent of doctors believe prior authorization is often unreasonable.
“Intrusive oversight policies that require physicians to get insurance company permission before providing care can delay patient access to medically necessary services,” said Steven Stack, AMA president, in an email. “The AMA continues to urge health plans to limit the application of prior authorization policies, or consider alternative approaches to control the cost of services and medications that reduce burdens on both patients and physicians.”
104 responses to “HMSA pre-authorization policy delaying critical tests, some doctors say”
Leave a Reply
You must be logged in to post a comment.




Shame on you HMSA. We pay our monthly premiums on time and expect the service we deserve. Thank you for shedding light on this issue.
Not a problem. New state law holding both HMSA and National Imaging Associates legally and financially liable for any health issues/medical damage caused by delayed processing.
Both responsible to cover medical costs, pain and suffering damage to injured patients.
$2000.00+ A Month for a family of 3 persons is ridiculous and then they want to delay and approve in advance the doctors
tests. Thanks to Obamacare ( ACA)it now takes 30-45 days to see a doctor. Prior to Obamacare (ACA) the monthly premium was $1200.00 and we could see a doctor within 2-5 days so tell me how this has helped those who have insurance. Thanks to the Democrats of Hawaii and those who elected Obama we the people who actually work and pay taxes now get to suffer. We are lucky they have PA’s because that’s all your going to get nowadays.
This issue has nothing to do with Obamacare.
Everything in health care today now is a consequence of Obamacare. That was the whole point–to put the government in a leading role for all aspects of health care. Obamacare effectively requires cost controls such as pre-authorization to prevent plans from becoming “too expensive”. The government is more in charge of the process than you are, so the insurers weigh their response to placate the government vice the consumer. It’s exactly what democrats (primarily) asked for.
That’s not true. Pre-authorizations have been around forever; just like HMO referrals.
Dolphin, here is a link from HMSA Quest pre-authorization from 1994, last I checked that is well before Obama took office.
http://www.hmsa.com/PORTAL/PROVIDER/zav_QI.01.PRE.10.htm
here’s an article that says “HMSA’s preauthorization process has been in place for more than 10 years.”
http://www.staradvertiser.com/editorial/preauthorization-protects-health-safety-of-hmsa-members/
Isn’t it better to have a patient get prompt testing and treatment then give kala to his/her grieving family because HMSA’s profit over care business is given free reign?
Yes, however, your worst case scenario is not typical. Pre-authorization, like the article says, exists to prevent fraud by doctors looking to make a quick buck by ordering unnecessary tests. Without pre-authorization, what is the incentive for doctors to be honest in this regard?
The doctors ordering tests don’t make money. The testing lab or facility and it’s staff do.
Doctors order tests for two reasons:
a) it can help better understand what’s wrong and what treatment to provide to reduce patient suffering, disability and death from illness and injury.
b) to cover their butt from any lawsuit that they failed to do enough tests to achieve (a).
Doctors order tests to thoroughly evaluate patients. If they don’t order tests and something bad happens the physician gets sued. So how does this pre authorization help the physician and patient?
The responsibility for this insanity lies squarely at the feet of Obama and the Democrats. Their scam; to provide health insurance for 40 million Americans, was just that, a scam. The scam was supposed to provide health insurance, but has succeeded in destroying “health care” in America. You may ask yourself; how could they have gotten it so wrong? How could a plan to insure more people get so screwed-up? Answer: Obamacare is the con of our lifetime. It was created to become an incredible problem, that the folks would demand the government solve. Solution: Single payer, or socialism. Thank a Democrat for turing the USA into a mess. They, along with Obama, have been and are, the most dangerous threat facing our country. Far more than ISIS.
O B A M A curse is alive and well. ANYTHING he touches turns BAD..from Solyndra to Tiger Woods to Foreign/Domestic Policy to the Economy to America’s HEALTHCARE system.
Obama has nothing to do with this. This is an insurance company ploy…although, I will say that there are doctors who, as the article cited, would abuse the power as well.
This is neither an Obama ploy or an insurance company ploy. Fact is most if not all insurance companies require pre-authorizations. HMSA was just late getting to the table and consequently receiving backlash from their provider network accustomed to doing things the old way. Pre-auths are routinely denied for lack of information but once the provider submits the necessary info, a decision gets made. A provider can submit the pre-auth as urgent or appeal a decision if it was denied. Unfortunately, this does require more effort and staffing on the doctor’s part but increasing health care costs has led to this. If I were considering becoming a doctor, I’d become a veterinarian instead – much less red tape.
d, Point taken. Question, your sentence beginning with “Unfortunately” isn’t it the increase in staffing that causes the increase in health care costs? Sorry, maybe I’m misreading. Totally agree though, veterinarian is the way to go, cash money.
Your wrong Obamacare has everything to do with this & it’s only going to get worse.
Sami, please explain?
You’re either extremely naive, or you haven’t bothered to read the ACA, like most. The worst of this nightmare hasn’t even surfaced. Obama made sure that wouldn’t happen until he’s out of office.
Peanut..how about some details?
Peanut, please see my links above. Again, pre-authorization has nothing to do with Obamacare.
@advertiser1 “unfortunately” relates to the fact that doctors have unfortunately had to increase their clerical staff just to deal with the myriad requirements related insurance billing/claims, Medicare/Medicaid regulations etc. This relates to the cost of doing business to run a private medical practice these days which is a drop in the bucket compared to the rising cost of health care treatment as it relates to expensive tests, medications, durable medical equipment, hospitalization, emergency care, etc.
d, that’s what I thought. Thank you.
Out come the tin foil hats. The fact is that, because of Obamacare, this patient can’t be denied health insurance just because he survived a quadruple bypass. Because of Obamacare, this patient won’t go bankrupt from a jacked up healthcare premium for a pre-existing condition. Because of Obamacare, millions of Americans who were previously going without health insurance, now have it. Healthcare costs were already skyrocketing under the previous GOP presidency. This is simply, and solely, a money grab by the HMSA CEO. His pockets need to be lined a little more by Hawaii residents, but he needs to find that “gold” somewhere.
This is all THEORY, HIE. What you say is what Obamacare is SUPPOSED to do. There’s no evidence yet that ACA’s goals have been achieved. ACA was proposed under the premise that there would be a single-payer fund. THAT PART never made it into the final ACA bill. And that’s the single biggest reason Obamacare is failing today, tomorrow and beyond.
How many people need quadruple bypass surgery? The rest of us who have taken better care of our health do NOT benefit from Obamacare. Our insurance premiums have only gone up, UP, UP!!!
All it is going to do is drive up costs with everyone going to the emergency room instead of getting these tests done by their doctors. HMSA thinks about the bottom line, yet they don’t even realize that this probably is going to hurt them instead of add to their bloated profits.
BAKER WANTS DOCTORS TO HAVE ACCOUNTABILITY WITHOUT AUTHORITY
The following quote is from the Star-Advertiser:
begin>>>
House Bill 2740 as approved by the state House would have prohibited health insurers from requiring pre-authorization that causes “undue delays” in patient care, and would have made the insurance company legally responsible if any patient injuries were caused by pre-authorization delays.
“There have been too many cases that have stretched out for four or five days and longer — several weeks in some cases. You don’t get good outcomes when things are delayed that long,” said Christopher Flanders, HMA executive director.
However, Senate Commerce, Consumer Protection and Health Chairwoman Roz Baker announced she was rewriting the bill so that HMSA’s pre-authorization process can continue. The new draft will specify that “nothing in this measure shall be construed to prohibit use of pre-authorization for medical treatment and services, or conflict with current contracts,” Baker said. “So there is no question, we are deleting the liability provisions in this measures, as the chair indicated she would early on,” Baker added, referring to herself. “This is the best the chair could do given all of the moving parts, but we’ll see what (the Judiciary Committee) has to say, and what other people have to say” after they review the new draft.
< << end http://www.staradvertiser.com/hawaii-news/senator-to-alter-bill-to-give-hmsa-a-pass/
Before Baker broke the hb2740, its main goal was clear, and it was this: whoever has the authority to decide about whether or not a test is performed in a timely manner should be responsible for this decision – this means legally responsible. To seize authority (that’s what authorization means) and then to shift responsibility onto others can be irresistible for those with power and influence, but this won’t lead to better healthcare (or to better governance, for that matter). It’s just not right, but it aligns with Baker’s misplaced priorities – protecting big business, not Hawaii doctors and patients.
As Kristen Consillio reports, Dr. Christopher Marsh has to employ 10 people to do the administrative work for only two doctors. “They are on the phone or the fax all day long trying to get our patients approved medications, imaging tests, referrals, etc.,” Marsh said. “My beef is that this micromanaging of my day-to-day patient care is trashing my ability to take care of my sick patients.”
I learned last week that Hawaii will be losing Michael Castro, one of our best oncologists because his busy practice couldn’t pay the bills. Dr. Castro cared for my dying Dad two years ago, and even though he was just the consultant when my dad was admitted to Queen’s, he was the most compassionate, competent and available doctor on the team. (BTW, the QMC doctor in charge was a shocking disappointment.)
Dr. Castro is headed to the mainland and Hawaii now has one less competent specialist who actually provides clinical care. Meanwhile our health plan doctor networks that are already inadequate, are getting worse. Due to lack of competent oversight by Maui state senator Roz Baker, the DCCA Insurance Division is not enforcing the laws against this. So plans just keep harassing and squeezing doctors like Castro. Dr. Castro said he had to pay 6 full time staff just to fight for approval of tests and treatments and although the requests were almost always approved in the end, it was just too disruptive and costly to jump through all the hoops that he couldn’t stay in business. It is ironic that Baker has pushed for funding of the UH Cancer Center, where she has close personal ties to the leaders, but won’t lift a finger to help the practicing oncologists our cancer patients depend on.
Roz Baker has done nothing to enforce the laws requiring health plans to have adequate physician networks, so plans are able to continue operating in ways that drive Hawaii doctors out of practice – and they do so with impunity. The plans don’t mind because fewer doctors means less care, fewer claims, less payments and more profits.
What other private industry in Hawaii is allowed to promise consumers access to an essential service (one it is legally required to provide them), to accept payments for this, to regularly fail to deliver, and to top it off keep the payments with absolutely no consequences?
Baker admits this happens, but then does nothing. Insurers have over $6-billion in annual revenue but they are not being compelled to do anything to maintain their participating provider networks. No wonder they love Baker. Other states monitor and enforce health plan provider network adequacy, and in those states health plans are forced to invest in doctor recruitment, relations and retention. If not, the plans are fined.
Hawaii taxpayers give two of the for-profit mainland companies over a $billion a year to care for Medicaid members. These plans, Ohana-Wellcare and UnitedHealth Care, paid out approx $200 million/yr less than they received from taxpayers, giving most of this to out of state shareholders and greedy executives. At the same time, many of those covered by these oppressive mismanaged plans can’t find a doctor willing to care for them. To make matters worse, the untreated health problems of all these poor people make it harder for them to work and care for their families, resulting in even more state expenditures for unemployment, CPS, EMS, public safety, courts and corrections, homeless programs, state hospital and DOH. The county also has increased costs, not to mention the human costs and strain on families and communities.
Baker’s primary concern regarding access to care this session has been access to Medical Marijuana. Not only has she championed several bills, she even held special hearings and vigorously challenged the health department. Baker clearly knows about her oversight powers:
“I get very frustrated when executive departments establish rules that go beyond what the Legislature opined,” Sen. Roz Baker (D, West Maui-South Maui) told health officials who testified in front of a joint hearing of the House Health Committee and Senate Commerce, Consumer Protection and Health Committee. “The Legislature makes policy and the executive branch implements that policy. So I would like you … to look at those rules and in areas where they go beyond what the statute says specifically, take them down. They don’t belong there.” (Star-Advertiser)
So why then, has Baker chosen NEVER ask why neither the Insurance commissioner or the Director of DHS have followed the laws requiring them to ensure that health plans maintain adequate provider networks? This would force Hawaii health plans to stop driving our doctors out of business, and to come up with sensible ways to improve access to safe, effective and cost-efficient care.
This session, Baker even refused to hear a no-cost, common-sense bill (sb2287) that would have informed health plan members of their legal right to an adequate provider network, and that would have required health plans to maintain accurate directories of participating providers. This bill was based on the NAIC Model Law. Senator Chun-Oakland had introduced this bill, it was presented to Senator Bakers’ head clerk and discussed in detail before the start of the session when they were provided two hundred pages of supporting documents. Mid-session, Baker’s clerk said the bill would not get a hearing.
When asked about this on March 3, 2016, Baker replied, “At this stage in the session we’re constrained by what has already been introduced and topics discussed.” Baker was reminded that the bill had been discussed with her staff, presented on time and was sitting before her committee, and she was urged to give it a hearing. Baker did not respond.
The bottom line is that Roz Baker has time to meet with the insurance industry and to hold hearings to demand patients have access to Pakalolo, but has no time to push for access to real health care.
Baker’s actions on hb2740, making the physician responsible for the clinical decisions of health plans and promoting onerous administrative hassles, fit her pattern of protecting the interests of big business rather than consumers. If the Senate was being honest, it would rename Baker’s committee from “Health and Consumer Protection” to “Patient Exploitation and Industry Protection”.
You can be sure Baker is working hard to protect HMSA right now.
Since you’re Sen Roz Baker bashing I thought I would contribute a story.
Legislation to airbnb Senate Bill 2693,
introduced by Sen. Roz Baker, D-Maui, would allow alternative accommodations
companies to register as tax collection agents with the state.”
“If passed, it would create a mechanism for such companies to collect and remit general excise
and transient accommodations taxes on behalf of the host and visitors that use
their platform.”
I hinted if she could introduce legislation for all those small business owners
who currently collect GET from their clients/customers as a form of credit/compensation.
Small business owners are in effect Tax collection agents that don’t receive any credit/compensation to maintain a
database of clients/customers to collect these taxes on a quarterly basis. There are associated
costs ofpostage/envelope, sending payments to the state tax department on a quarterly basis
utilizing small business personal stationary/checks (They get penalized if payments are late.)
Baker responded, “As far as I know, no one gets a credit for obeying the law”.
It’s all about the money, profit versus patient care.
Its all about personal responsibility now. Take care of yourself. Because the system won’t.
https://www.youtube.com/watch?v=30gEiweaAVQ
No kidding. Their response to Wong makes it clear:
“The insurer contends that Wong did not submit the medical records required to get the heart scan approved, did not tell HMSA the test was urgent and did not take advantage of an appeal process in a timely manner.”
You shouldn’t let a patient die just because he didn’t go through all of your BS red tape.
“HMSA has asked that we tell you that — to a certainty — any implication that those patients were harmed by HMSA’s preauthorization requirements is false and defamatory,” Alston wrote. “If you do not immediately notify the media that these allegations are false, you (and anyone else involved in disseminating these false claims) will cause serious reputational harm to HMSA. Please be aware that HMSA is prepared to pursue its legal remedies to address the harm caused by publication of these claims.””
“…seriousness reputational harm to HMSA” Come on HMSA, your reputation is so bad by now that bully attics such as this only serve to tarnish it even more.
I forgot to say, “SHAME ON YOU HMSA FOR TRYING TO BULLY THE DOCTOR!”
I regularly see my doctor and my doctor orders labs before each visit, HMSA has access to those lab results; so they know how my health is doing. The pre-authorization is unnecessary. I see the cardiology’s point of view, if you have a patient that is requesting to be seen more often, then there is something wrong.
If you are a soldier (doctors) and on the front line and can’t fire your gun without preauthorization from an officer miles away (HMSA), you are dead. Sure, some soldiers may shoot unnecessarily but it doesn’t mean you handicap the whole batallion.
This is HMSA watching their bottom dollar. Dr. Cogan just earned a gold pass for his supporting HMSA comments.
Very astute comment!
Agreed.
True story: A few years back, my Dad went to see Cogan for an arrhthmia, and the first thing Cogan wanted to do was Angiography, which is expensive and dangerous. When told about the possibility of death from the procedure, my Dad asked if the test was necessary and Cogan said “probably not” and he was unable to give a compelling reason for it. My Dad refused, and Cogan ended up just refilling the medication he had been on for years. He never trusted Cogan after that. My Dad’s heart was fine until the f——g lung cancer claimed him (don’t smoke!).
I heard from other doctors that Cogan is an interventional cardiologist (AKA a cath cowboy), so it is curious he is defending HMSA’s draconian bureaucratic hurdles.
Perhaps, as you suggest, it means he will be getting the green light more often for his authorization requests.
Too bad we don’t have better choices in health plans. Next open season, I will look into other plans available as HMSA has forgotten the word “member” and does not represent us as they should. Even calling them for assistance is like going nowhere and you meant to feel like you are bothering them. Auwe!
HMSA has a sweetheart deal with National Imaging Associates Inc. Willing to bet there are kickbacks and bonus payments for ever disapproved request. Talk about 10th world medical service.
HMSA bureaucrats are throwing up walls of Red Tape in requiring volumes of medical information, special requests, anything to make the approval process harder, not easier.
To be fair, all pay raises and bonus payments for HMSA management bureaucrats will now go through a member/patient review and approval board. All requests submitted one year in advance, 25 copies, complete job performance review and board interview will be done prior to any approval. Zero tolerance for mistakes, no pay raise or bonus. No need to waste money on utterly incompetent bureaucrats.
Good for the goose, good for the gander.
10th world now, down from 8th world.
Please tell us all how you know there are kickbacks for disapproved requests.
Again, and I’m so sad that you never respond, how can you have so much contempt for those you call bureaucrats when you yourself were one?
I say, SUE HMSA big time. If they want to save money on patient’s lives, then have them pay for negligent.
Totally agree.
HMSA-busted.
I also see a class-action lawsuit from the physicians coming against HMSA, including for not answering those questions posed by the newspaper. Lets see how that saves them money. Oh wait, they would just raise our rates to pay for their legal costs! So at 10:00 pm in the Arizona (7:00 pm Hawaii time) a physician screener in all specialties is available to review urgent cases over the phone? Could a MD who is a urologist by training working the night shift be making decisions about your brain scan for a tumor by your neurologist?
Maybe it’s called “Human Depopulation”, if your going to ignorantly eat radiated fish as if there never was a fukushima accident, and then expect expensive life-saving treatments and testing, for health related illnesses, then what’s the purporse? You get this expensive surgery, and then the first thing you want to eat when you get home is radiated raw sushi?? They should give patients a rad reading first as a means of testing. .
What?
Smokin’!
Shame on HMSA. Glad you published Alston’s letter. Why not spend money on patient care instead of threatening to sue.
It’s kind of funny that everyone is roasting HMSA as they try to control cost and save money but when HMSA raises their rates, these same people are crying foul. I guess HMSA can’t win either way haha.
Are they trying to control costs or increase their margins to the demise of the patients? Before HMSA raises rates they should look at their own bloated overhead, contracts, and management staff. While the rest of the business world does more for less, HMSA does less for more. Who oversights this near monopoly?
Exactly. I’ve been getting survey forms from HMSA for so many times after seeing a doctor. At first I diligently filled them up and mailed back. Then I realized that it’s basically useless. So I stopped, but they kept sending my way. I wonder what those statistics work will do to improve patient care, other than keeping the jobs in their stats office.
In 2013, the Hawaii Medical Service Association raised the pay of its chief executive Michael Gold by 19 percent to $1,300,000.00/year. Wonder how much more Mr. Gold get’s paid this year?
Greedy Mr. Gold… think about it.
Why is this profession still using fax machines? Scan it to create a PDF and email it with proof of delivery. Now you have a record of what was sent and easy to re-send it when they inevitably tell the doctor “Oh, we didn’t get it”.
C’mon guys, the 1980s called and they want their fax machine back.
Funny that you said that because I was thinking the same thing.
I also wondered why Dr. Wong didn’t put in the requests in February … or previously if his patient’s heart was so totally blocked. How can you “care for” a patient for 11 years and not know that his heart is almost totally blocked? Sounds like the doctor is above and beyond following rules … and thereby will never be gold carded.
This has to to with Federal regulations (HIPAA), another layer of regulations strangling doctors, which allows transmission of medical information over phone lines, but not via eMail. Go figure.
Maybe Schatz and Hirono can fix this for us? Not likely with our do nothing Congress.
Thank You Star Advertiser for the article. I will hang it up in my 2 examining rooms so that my patients can understand why its taking so long to get an approval. I understand what HMSA point of view but it appears they have no clue what really happens when we need to get a pre-authorization. I enter all the important info, and 99% of the time, the response is “pending”. Then a day later, I get a reply that states need records to verify request. Why fill out the form when I know 99% of the time the computer is programmed to say, “pending, need more info”. Why go through all the time consuming initial request? Just send the records ( Dr. Cogan know that) How do I know its programmed that way? I’ll give u good example. I finally got an approval to have a pt do an MRI. The pt thanked me, but requested if he could do it in another facility which had an open MRI because he suffers from claustrophobia. No problem right? Wrong! So I requested a change of venue and explained in box that is provided for all request. Guess, what. The reply was as usual “pending, need more information,. please send medical records, consult reports…..” Then I knew for sure, the computer is programmed to almost always say “no”. I doubt there is a human mind that is reviewing all initial request. If any HMSA MD is reading this, I bet you if you did the same thing I did, you’ll get a denial. Its programmed. Sad.
All these requirements adds additional work to doctor and staff. Add it to Medicare/Medicaid data gathering and it lengthens time to each visit, so docs are running behind schedule. Got a letter from HMSA regarding new payment plan for physicians where doc(s) will be paid a sum of $$ per month no matter how often I see them. Is that better for the doc and the patient? My doc is so frustrated that closing the practice is VERY REAL. Can HMSA find me a new doc?? I doubt it – try asking someone who has tried to find a new doc that will take them.
Hawaii health plans driving doctors out of business until our laws start getting enforced by the insurance commissioner:
HRS432-f(2): “[Commercial managed care plans] must provide access to sufficient numbers and types of providers to ensure that all covered services will be accessible without unreasonable delay, after taking into consideration geography.”
HAR17-1735.2-4: “[MedQuest plans shall include] development and maintenance of a sufficient network of health care providers to ensure the provision of required health services are provide to an eligible individual in a timely manner.” This requirement is also present in federal law (42 C.F.R. 438.206).
Guess who is in charge of oversight of the DCCA Insurance Division? Senator Roz Baker of Maui, loyal friend of the insurance plans, not the doctors.
Why was the Senate’s only physician, Dr. Josh Green, kicked off the health committee last year, and Baker named chair of the new Consumer-protection/Health committee? Oh yeah, because access to Pakalolo was more important to our Senate leadership than access to medical care.
Mr. Gold is laughing all the way to the Bank and Roz Baker is raking in the political donations from the cannabis lobby and the health insurers, while We the People keep paying ever rising insurance premiums and more more of us can’t even find a participating doctor.
I don’t think this has much to do with Obamacare, just plain lust for power and money.
Obama supporters see no connection to Obamadon’tcare, but there is a connection, Obamadon’tcare is a gift to the medical insurance companies, and it protects them from losses. However, in this case, it is the corrupt Democrat Party in Hawaii that has leveraged tremendous power to Hawaii based healthcare insurance companies especially HMSA. With virtual monopoly power, they will bully the medical community, lower the standard of care, to the point that the Hawaii patient doesn’t know any better or has to pay out of pocket or go to the Mainland to get the needed treatment or both. This is plantation mentality, one party rule corruption that Hawaii has to suffer through because of deception and ainokea attitude.
Except that HMSA wielded this kind of power prior to Obama.
Yeah, HMSA was a “virtual monopoly” long before so called Obamadon’tcare. THe rest of Maipono’s points I agree with:
a) Our corrupt/incompetent political leadership that persists because of a lack of accountability. (This could be due to one party-rule, but I’m not sure.)
b) HMSA dominates the medical community, which has little power or influence. If might makes right, then I guess it’s all good.
I guess because the Democrats have dominated here for so long (Lingle aside), that it’s hard to find examples of Republican corruption. But, there are many cases on the mainland, so logic would tell me that it’s not related to a party, but just the nature of the beast.
Guess what there is an cure for Heart Disease but illegal because not approved by the FDA. But there is a US patent issued for it.
HMSA is practicing medicine w/o a license.
Great article
If this dr Cogan knows of doctors that own their own MRI and are making money off pushing unnecessary tests, where is this please? I think that’s Hmsa b.s. But let’s hear specifics
Hmsa is running out of room on this
Doctors pay a lot of unnecessary staff time and therefore money to satisfy the Hmsa computers, then more again, to have staff re chase records
This will lead to less and a lot less physicians practicing in our state because these are direct costs to our physicians
And then Hmsa will pay those remaining physicians less money every year in their new program, to care for each of us. Again, running our physicians out of Hawaii. They won’t be able to afford to practice
Spot on, localcitizen. We should all think about this next time we get only 5 minutes with a burned-out doctor.
It’s getting to be like the Woody Allen complaint, “The food here is terrible, and the portions are too small.”
And sum this all up
Our premiums have gone thru the roof
Our physicians are making a lot less, now pushed to make less by caring for more of us
Tests that our physicians used to be able to order to see what’s wrong with us, are now being denied
Physicians are going to leave, we won’t get better care this way
And
Hmsa is collecting more and more and more every year
If it isn’t going to physicians, or care, ,,,,,where is all this large e try money going??
And don’t say that somethings wrong with Hmsa, or you’re going to get sued!
This whole situation is Dr. Mugiishi and CEO Mike Gold’s fault. These two crooks along with the rest of HMSA’s board need to be replaced because they are putting patient’s lives at risk by delaying scans and (from yesterday’s news) encouraging doctors to see their patients as little as possible if they want to get compensated adequately. I remember when HMSA was the gold standard for medical care in Hawaii. Since these two have been at the helm, they have sold out to the mighty dollar and have started to make decisions that are contrary to their core mission. They’re supposed to be a non-profit, but now they sure act like a for profit health care organization. At this rate, people may want to go to Kaiser because at least Kaiser is really good at keeping you healthy and if a doctor wants an MRI or a CAT Scan done, you can usually get it done very quickly without requesting an approval or dealing with red tape like the doctors that deal with HMSA go through.
Am thinking Gold brought Mugiishi in to save HMSA. Mugiishi has the respect of the community and integrity. Gold does not. Making Mugiishi the ‘fall’ guy
agree about going to Kaiser – no delays and no pre-auth
HMSA playing God!
It’s been 48 day’s and I am still waiting for my pre-authorization for heart med’s. My doctor has been giving me samples to keep me from having a stroke. Thank you HMSA or OBAMA witch ever-one is responsible for playing Russian roulette with my life. And for putting brand name drug’s on a tier program that does not allow us on Medicare from having.
An older friend of mine is trying to get approval for Hep C treatment. They will not approve his treatment until he reaches Stage 4. I guess they prefer someone to die first!
That is actually incorrect. HMSA will approve Hep C treatment when you reach Stage 3. Anything below that, even if you are .1 below the Stage 3 threshold, they will not treat. Kind of dumb that they won’t treat Stage 2, but it all comes down to the bottom line. Have your friend go to Queen’s Liver Center. If he is Stage 3, they will get him treatment.
That said, I do not like HMSA’s pre-authorization policy as it held off some very important tests for me as well. They will make you do a cheaper test, then when your doctor isn’t satisfied with the test, they will approve the original test. To me, that is a stupid waste of money. Paying for 2 tests, when the more expensive one would have sufficed.
Roz Baker is nothing but your typical politician with her hand out. Not surprising as she was a well heeled Washington lobbyist before she saw greener pastures here in Hawaii.
Boy you guys on Maui are really lucky having her represent you. Along with Joe Souki, Kalani English and Alan Arakawa, you can all go back to sleep. Lucky, yeah.
Since you’re Sen Roz Baker bashing I thought I would contribute a story.
Legislation to airbnb Senate Bill 2693,
introduced by Sen. Roz Baker, D-Maui, would allow alternative accommodations
companies to register as tax collection agents with the state.”
“If passed, it would create a mechanism for such companies to collect and remit general excise
and transient accommodations taxes on behalf of the host and visitors that use
their platform.”
I hinted if she could introduce legislation for all those small business owners
who currently collect GET from their clients/customers as a form of credit/compensation.
Small business owners are in effect Tax collection agents that don’t receive any credit/compensation to maintain a
database of clients/customers to collect these taxes on a quarterly basis. There are associated
costs ofpostage/envelope, sending payments to the state tax department on a quarterly basis
utilizing small business personal stationary/checks (They get penalized if payments are late.)
Baker responded, “As far as I know, no one gets a credit for obeying the law”.
Dr Wong is a great cardiologist who is proactive in his approach to healthcare. I have gotten a number of imaging test done by him in the past that gave me a baseline of the condition of my heart. We would routinely do a test (every two years) to check. Now we do have to jump through hoops to get that testing done. If I get a heart attack it would cost HMSA more in my healthcare then this routine test. Health care insurance is really screwing themselves up because instead of being proactive, they are reactive and by then it is too late. The medical cost would be more to fix the problem.
Both sides of this equation are culpable.
HMSA just didn’t realize that this procedure may cause a lot of staff and physician time and stress to save them a bit of money. The patient will be delayed and have to make at least another trip back to the doctor’s office to get the approval and be scheduled for the test. Along this path, mistakes can happen and everything can go wrong. Whom to blame?
Save “them” a bit of money? Actually, the them is YOU. HMSA is constantly trying to reduce costs to minimize your health care costs. It seems that a lot of people don’t see the whole picture and will grumble about all efforts to lower costs. Bottom line is that your medical bills won’t climb higher than it needs to be. If you can find a better plan at a lower cost, then you should go for it. I know that I can’t.
Please then tell us
Amount of subscribers increase over last 3 years
Amount of increase in premiums overall, then per subscriber past three years
Now you say Hmsa is really working for us?
Increases in Hmsa administration, not to healthcare providers
Increases to Hmsa executives
Oh,
And let’s too in Political Contributions….and exactly how much and to whom
Bet you your Hmsa supportive theory falls flat after you get real data
They are paying themselves, their pals, not the healthcare providers
save money for us subscribers?? Lol
Do you work for HMSA or have some type of vested interest in them Readitnow? You seem quite defensive. Anyway, I”ve been a long-time HMSA subscriber but I’m in the process of switching over to Kaiser because HMSA’s premiums are just too expensive for me. Kaiser is far more affordable and their customer satisfaction ratings have been decent. And no, I do not work for Kaiser or have any vested interest in them.
I’m a retired accountant that never worked for HMSA. All I know is that HMSA is a nonprofit that charges customers to pay out their medical bills with a little more to cover their cost to run the company. If charges to patients go up, then insurance rates will go up.
If going to Kaiser is best for you, then you should make the change. I’ve worked for companies that did change insurance plans, but we always made the change back to HMSA. Do what is best for you.
To make the picture clearer … I understand that premiums are climbing really fast. In my case, I’m also a disabled veteran that is covered by the VA. So, I don’t have many of the costs that you face.
My defending HMSA is more that I see a lynching mob forming. I just wanted people to step back and see the whole picture. Good luck to you akkman!
One of the two of AMA suggestions is to ” consider alternative approaches to control services and medications that reduce burdens on both patients and physicians” seem a good venue to help solved pre-authorization policy!
HMSA looks pretty bad on this but unfortunately like they said, this whole thing happened because of doctors who order unnecessary tests to make money. If we could trust doctors this wouldn’t be a problem. Unfortunately there are plenty of doctors out there looking for ways to make extra profit. But I feel for the doctors too, it’s a lot of pressure to keep their practice alive. It’s all part of our lame health care system. Kaiser has fixed some of these problems by paying doctors a salary, so they do not have incentive to make profits with unnecessary tests or seeing extra patients. I’m not saying all doctors are doing this but many are.
Exactly, and that is why HMSA is reviewing the doctors and giving out gold cards again. If I read correctly, when the doctors pass review and receive their gold cards, then they won’t need to get this preauthorization. Same as what was done previously.
So Docs … quit making waves and you will have your gold cards back.
Why was HMSA not already collecting and analyzing data on physician ordered procedures? They should know who the so call outliers are and take action on them. Not punish everyone by taking their gold cards.
” Order unnecessary test to make money” How is that?
HMSA:
If you want to reduce the number of tests ordered by a significant percentage, lobby for responsible tort reform.
Concern about a lawsuit motivates physicians to cover every base, no matter how unlikely.
Grover LIese M.D.
My doctor used to say “I HATE HMSA!” so vehemently and I can understand why.
A couple of my doctors have also expressed hatred towards HMSA. I’m concerned that we will see an even larger shortage of doctors wanting to practice in Hawaii because of having to deal with HMSA. We already have a shortage of doctors in certain specialties and it’s sometimes difficult to get an appointment.
You got that right berniel1, Hawaii already has a severe physician shortage and HMSA’s latest ploys will not help the situation. Maybe some of them will give up and move to Kaiser?
Even if legislation is passed putting liability in the insurer’s lap, the attorneys and bean counters will find a way to 1) Get out of their responsibility completely through the “legal process”, and 2) Hike everyone’s premiums up to cover increased retainer fees and build up a cash supply to fight any future legal entanglements. Please note that the review company issued a letter to the doctor making the request from their ATTORNEY. THE HEAD OF CARDIOLOGY AT THE STATE’S BIGGEST HOSPITAL BEING THREATENED WITH LEGAL ACTION FOR EXPRESSING HIS VIEWS. An individual who, in all probability any shyster would want as an expert witness for the depth and breadth of his experience and knowledge in the medical field…think about how crazy that is!
Went to ER with chest pains and shortness of breath but was released within a couple hours. Because of my history of Diabetes, Heart Disease, Previous 75% blockage in Coronary Artery requiring a stent the Nurse Practitioner for my cardiologist ordered an angiogram. It was quickly denied. They say I am borderline for a heart attack and cant take Motrin or Aleve to help with the pain because it can actually trigger a heart attack in people with my history. Now I am taking Vasodilators (not fun) again and waiting for Nuclear Stress test. Still have intermittent tightness in my chest but still waiting to see what happens next.
There has got to be a better way. You can’t afford to tip life-and-death situations the wrong way. Some practices of the insurers are downright shameful. Insurance companies must stop being so disingenuous.
I am going to cancel HMSA when open season occurs for Federal Workers this year. I will have the same coverage under TRICARE. I opted to pay for HMSA because I felt the service was better. Now it is the same so I’m going to save several hundred $$ per month and just pay for my TRI CARE.
HMSA by creating more requirements and red tape for critical tests while simultaneously continuing to raise their premiums higher and higher is sadly alienating its customer base away, at least that is my personal case. I’ve always loved the HMSA network of physicians and enjoyed the freedom of choice that their network provides. However it’s gotten to the point where I can’t afford their monthly premiums anymore, especially with their 90/10 plan (which even with employer contributions, I’m paying almost $1,000 per month for a family plan). With kids soon going to college, I just can’t afford this anymore and I’m forced to consider alternatives, such as Kaiser and I’m switching over during this enrollment period. The Kaiser plan is much more affordable and they actually have decent customer satisfaction ratings. Well, I hate to leave some of my HMSA physicians, especially our really good Pediatrician (Dr. Kandasamy) but I feel I have no choice.
Side note: Yes, Obamacare has nothing to do with HMSA’s recent actions, however, Obamacare has forced my family to enroll in the prescription drug program (which was previously optional) if we wanted medical coverage. My family rarely uses prescription drugs and now we have to pay $300 more per month for a plan we don’t want or need.
You sound like a very good pt akkman. I have been in practice here in Hawaii for over 20 years. I do like HMSA. HMSA like all business are looking ways to cut unnecessary cost and increase profit for the benefit of many, including pts and MDs. They had good intentions and hired this group to screen imaging requests and deem if they are appropriate. The computer program that the company is using is not good. The qualitiy is not good. It does not reflect what HMSA is all about. HMSA has been in our lives, our father’s lives and even before that. I am hoping that HMSA will see that at correct it. I would hate to see HMSA and your doctor lose good patients like you. Us local Docs are very patient, so to see such an uproar from us, u know something not good is going on.
I guess we can still opt to pay for services…..
there needs to be a balance in healthcare cost – patient’s care and cost of care. this pre-authorization policy by hmsa is an attempt to contain medical care costs. hence, all sides (3) must work together to work things out. 3 =s, the patient, hmsa and the physicians. if costs are not reasonably contained, in the end the patients will suffer, both financially and care wise.
hmsa CEO makes too much money .
What about other health insurance like Ohana. Hawaii is all about wealth and health but what about the very poor seniors and disabled? Do we throw them in the dumpster after they die?
I will shed some light on this pre-authorization process. When it first got started, the physicians’ staff had to call NIA over the phone. The person who came on is an intake worker who knows nothing about medicine and would ask you all kinds of unnecessary question. When you get fed up with that person, he/she will pass you on to a nurse who would want all kinds of written medical records to justify your request. If the doctor thinks that this wastes too much of his time, he can bypass the nurse to talk to the consultant who used to be a retired doctor who had been in private practice himself and understands why the request was made and will approve it right away.
Then they came out with this “easier” online application they requires you to answer correctly what they want you to say. Any deviation in an answer will automatically generate a denial, and ask you for medical records to substantiate your request. With any rejections, HMSA will send you by fax a several page document telling you how to appeal their denial.
Please remember that with a SEVERE SHORTAGE of physicians in Hawaii, who will have the time to comply with all of HMSA’s red tape ?
Sometimes, the requesting doctor had to get the consultant’s name and tell him/her that if any harm comes to the patient because of their delay tactics, that consultant’s name will be given to the patient’s family for possible legal action.
Just because HMSA is the mighty Goliath, they can control the way that physicians have to practice medicine.
Again, let me emphasize that compromising the ability of physicians, especially those who have years of excellent track records, will not save HMSA big money. They should divert their attention to unreasonable price hikes of the pharmaceutical companies and high costs of hospital charges.
In a previous article in the Advertiser, some doctor implied that paying the primary care doctors less will improve medical care. What kind of reverse logic is that ? When socialize medicine start in 2017, solo practice and small group practice will have to close their doors for good when their income falls short of their expenditure.
GOOD LUCK TO FINDING ANY DOCTORS IN HAWAII IN THE FUTURE !
DON’T GET SICK AND DON’T GET OLD !